As reliable as joint replacement surgery can be, a variety of problems can occur which creates trouble for the joint replacement patient. We’ll go through a few of the most common issues and outline the general treatment algorithms below, but if you or someone you love is experiencing problems with a previously replaced hip or knee, we recommend a thorough in-person evaluation. Such a consultation begins with the patient gathering some critical information dating back to the time of the original surgery. The items we need include:
- X-rays from before the replacement and x-rays early (within a few weeks) after the replacement was performed
- Current x-rays taken within the last few months
- A copy of the operative note dictated by the surgeon
- A copy of the implant record (often called the “sticker sheet”) from the hospital where the surgery was performed
- Copies of office notes from the surgeon’s office

It’s important we receive this pertinent information before your consultation so we will be best prepared to answer your questions during your visit.
MOST COMMON HIP REPLACEMENT PROBLEMS
Dislocation
All hip implants, including hip resurfacing devices, can dislocate. Fortunately, the rates of dislocation are declining. Dislocations are termed either anterior or posterior, based on the route the ball takes to come out of the joint. The surgical technique used often predicts the direction of potential instability, but not always. If one of the anterior approaches to the hip is employed (direct anterior, modified Watson Jones, anterolateral, direct lateral), the risk of anterior dislocation after surgery is around 1% overall. The chance of a posterior dislocation is small if an anterior approach was used. Conversely, if a posterior approach is used (mini-posterior, standard posterior), the anterior dislocation risk is very small and most dislocations will be posterior. The actual risk of a posterior dislocation is dependent on many factors, however, if a capsular repair is done after the implants are placed, the chance is less than 1% both in our experience and as reported by others:
https://journals.lww.com/corr/Abstract/2001/12000/Effect_of_Posterior_Capsular_Repair_on_Early.19.aspx
The treatment for a hip that repeatedly dislocates usually involves revision surgery. In many cases, the position of the implants can be improved to prevent recurrent problems. Repairing the capsule and careful attention to postoperative precautions maximize the chances of success. If hip instability appears many years after a replacement, this can be due to major wear of the artificial bearing. Placement of a new bearing is the easiest revision operation to recover from. This being said, further dislocation problems do occur after revision surgery and sometimes require the use of constrained liner devices in which the ball snaps into the socket component.
Loose Implants
Sometimes implants that were originally solidly attached become loose, either due to cracking of bone cement or proliferation of wear debris. Early loosening of implants usually reflects failure of bone-ingrowth into porous coating, due to either inadequate early stability or poor bone blood supply. Intra-operative fractures can contribute to this problem, as can smoking and other health risks. Implant loosening requires revision surgery to correct the problem. If there is bone loss associated with the fixation failure, the surgery to correct the situation may be extensive and the recovery lengthy.
Leg Length Inequality
All patients should understand that determining and achieving equal leg lengths in total hip replacement surgery is not an exact science. Occasionally, the leg lengths are not exactly what the patient or we would desire. This is usually because achieving equal leg lengths needs to take a back seat to obtaining a stable hip. Our data suggests that we achieve leg lengths within 5 mm of being equal in 90% of our patients. When the leg lengths are not equal after the operation, it is sometimes necessary to wear a lift in the heel of the shoe. A lift is required in about 5% of cases.
Our record with leg lengths requires substantial preoperative thought as well as intra-operative wisdom on the part of the surgeon. At times, lack of planning and/or inexperience results in a noticeable discrepancy. This problem may be partially correctable if addressed early, but it is difficult to rectify after the passage of more than a few months. The conservative treatment involves the use of a shoe lift. If the opposite hip requires surgery, a leg length inequality can be solved at that time.
Corrosion and Cobalt Ion Release
Sometimes the metal implants used in hip replacements can release metal ions into the hip joint. Titanium is well-tolerated but some ions such as cobalt are not. The cobalt ions are picked up by the body’s scavenger cells and they become overly active, digesting tissue and bone inside the hip joint. Sometimes the damage can be extensive and irreparable. The primary symptoms are new pain and/or stiffness in a replaced hip. This issue has proven to be a major problem with metal against metal bearings, but it occurs with metal-on-plastic bearings as well if corrosion occurs at the junction between the metal head and the neck of the femoral component. Fortunately, excessive cobalt can be detected by a simple blood test and usually the problem is rectified by revising the metal head to a ceramic version. Dr. Dearborn has extensive experience treating this particular problem in patients with a variety of implant types and has presented our clinical research on this topic around the globe.
Chronic Pain
The cause of pain after hip replacement surgery, in the absence of problems evident on x-rays, can be difficult to find. Obtaining the history and careful physical examination in the office are very important in this situation. Infection is the first potential source of pain to rule out, which is typically accomplished via blood tests and removal of fluid for analysis. If infection is confirmed, further surgery is usually required. In many cases, initial removal of the implants is required in order to resolve the infection.
Other causes of hip pain in the presence of satisfactory appearing x-rays, include stiff uncemented femoral components and various soft tissue sources. Injection of local anesthetic and steroid medication into structures such as the iliopsoas tendon sheath can be both diagnostic and therapeutic. In some cases, tendons can rub over the edges of prominent implants, and revision surgery is required to remove the source of the impingement.
MOST COMMON KNEE REPLACEMENT PROBLEMS
Stiffness
In most cases, knee range-of-motion is improved after a total knee replacement. Patients who obtain less than 90 degrees of knee flexion are uniformly dissatisfied after surgery. Risk factors for postoperative stiffness include below average preoperative motion, intra-operative technical factors, and postoperative pain management difficulties.
The treatment for unsatisfactory knee motion involves further surgery. Scar tissue must be removed and in some cases the implants need to be revised. Evaluation in the office will be necessary to discover the cause of the poor motion which will, in turn, guide the treatment.
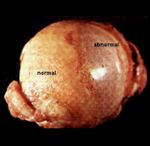
Bearing Wear
Over time, polyethylene bearings are subject to wear and potential failure. If there is no implant loosening or damage to the metal bearing, exchange of the worn liner can be the straightforward solution. In certain severe, chronic wear situations, metal against metal contact can occur, resulting in metal bearing damage and the shedding of metallic debris. Complete implant exchange is usually required in this setting, which often leads to bone loss necessitating the use of special revision implants.
Loose Implants
Sometimes implants that were originally solidly attached become loose, either due to cracking of bone cement or proliferation of wear debris. Implant loosening requires revision surgery to correct the problem. If there is bone loss associated with the fixation failure, the surgery to correct the situation may be extensive and the recovery more lengthy than for a simple liner exchange.
Chronic Pain
The cause of pain after knee replacement surgery, in the absence of problems evident on x-rays, can be difficult to find. Obtaining the history and careful physical examination in the office are very important in this situation. Infection is the first potential source of pain to rule out, which is typically accomplished via blood tests and removal of fluid for analysis. If infection is confirmed, further surgery is usually required. In many cases, initial removal of the implants is required in order to resolve the infection. Other causes of knee pain, in the presence of satisfactory appearing x-rays, can be elusive and difficult to treat. In some cases, tendons or ligaments can rub over the edges of prominent implants, and revision surgery is required to remove the source of the impingement.